No bread, pasta, vegemite or pizza, ever again – or at least, not in quite the way I remember it. Don’t even get me started on ramen because I may weep a little.
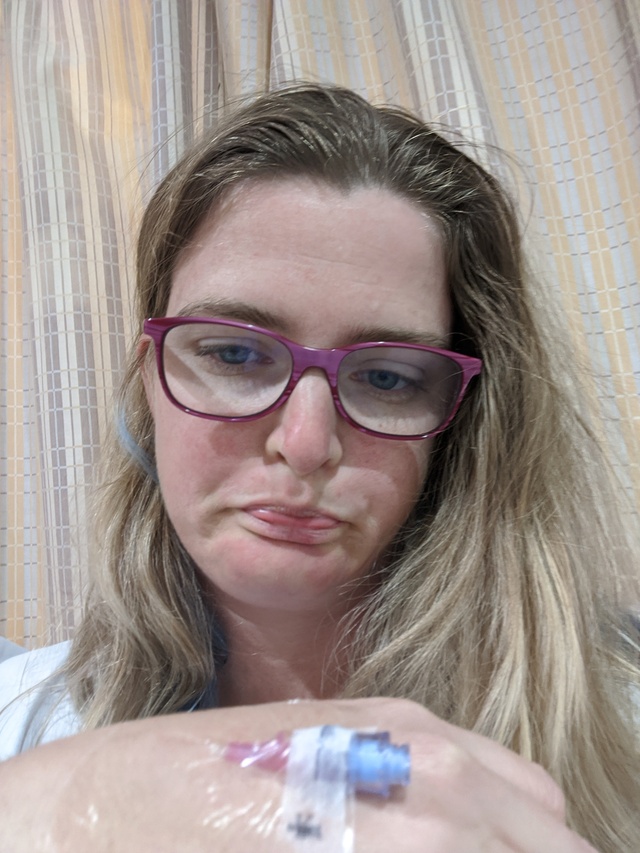
Coeliac awareness week has kicked off across the country from 13 to 20 March, giving the gluten intolerant amongst you (including Star Mail journalist Tanya Steele) the chance to highlight the challenges of living with the autoimmune disease.
To be short about it, no, Coeliacs cannot ‘cheat’ and have an occasional cheese toastie no matter how good they are – we beg you to please take it seriously because it has big effects on our health.
Often confusing for many, Coeliac disease affects thousands of Australians and around 80 percent of them remain undiagnosed.
The condition is triggered by gluten, which in turn damages the small intestine and causes systemic inflammation and it can lead to serious health complications if left untreated.
Shortly after my diagnosis in 2020 (yes – lockdown and a new diet regime, thanks universe!) over a phone call with a friend, I began to realise just how challenging coeliac disease was going to be.
I had been feeling very tired and run down and after a bit of back and forth with my GP and some blood tests, they had pointed to coeliac disease as a possible cause.
“A coeliac diet? That’s really hard,” said my friend.
My stomach dropped, Tatiana was vegan, and she was saying this was hard?
According to Coeliac Australia, Coeliac disease presents differently in each person, making diagnosis challenging.
“Some individuals experience classic digestive symptoms, while others have neurological, skin, or even fertility issues. Some experience no obvious symptoms at all but still suffer internal damage,” reads the Coeliac Australia website.
Symptoms in adults include ongoing gastrointestinal symptoms like diarrhoea, constipation, nausea, vomiting, flatulence/gas, cramping, bloating, abdominal pain, steatorrhea (fatty, floaty poo).
There are also effects like prolonged fatigue, weakness and lethargy, along with iron deficiency anaemia and/or other vitamin and mineral deficiencies, unexplained weight loss, mouth ulcers and skin rashes.
Children suffer with the disease as well, with symptoms like faltering growth or failure to thrive, persistent bloating and stomach pain, chronic diarrhoea and/or constipation, irritability and behavioural issues, unexpected weight loss, prolonged fatigue and weak tooth enamel or dental defects.
A friend has a son living with the disease, and she said overall he is pretty amazing about it all, and people are pretty good about being accommodating.
“It has taken time to get the school to come onboard,” she said.
“He very rarely complains about feeling left out but I know he worries about being different.”
“Or not getting an invite to something because it is too hard to cater for him.”
“As a parent you have to spend a lot of time and effort to make him feel included.”
One thing that was challenging is that you have to keep eating gluten until testing, eliminating or restricting gluten can make test results inaccurate. This means all your symptoms are still present – not fun!
Getting diagnosed is incredibly important because the disease can cause the malabsorption of nutrients and increase the risk of other serious conditions, including osteoporosis, liver disease, infertility, and certain cancers.
This basically means your body is not getting what it needs, and after an endoscopy and official diagnosis, I eliminated gluten entirely from my diet.
It’s not easy at first, there is a lot of learning around how and what you can eat. I would stay away from substitute gluten free products to begin with – it can be disheartening.
Instead, stay focused on the positives, what you can eat and what you enjoy.
The Coeliac Australia website states that the gluten-free diet is not for everyone and is not a ‘healthier’ way to eat (although the diet can certainly be healthy if managed well).
“There are nutritional risks associated with following a restrictive diet which must be carefully managed. A gluten-free diet is only recommended for those with coeliac disease or another medical need.” the website reads.
Gluten is in wheat, barley, rye and oats, although some coeliacs can safely eat oats. I had a few consults with a dietician to make sure I was on the right track, and I need annual check-ups and check-ins with my GP and gastroenterologist to monitor the condition.
Support from family and friends is very important.
If they are informed and aware, serving up communal meals means your friends with the disease can relax in your company instead of bringing a gluten-free protein bar as dinner to your BBQ.
Having a separate toaster and a clearly defined area for the ‘normal’ toaster, my family eat mostly the same as me with substitutions for some meals. Properly cleaning kitchen utensils and pots and pans is very important – any traces of gluten can cause a reaction.
Learning to read food labels and going out for dinner is a whole different learning process, but doable. Some really yummy places cater for gluten free diets, but a sneaky take away can be challenging.
I have found the Coeliac Australia website, online social media groups and fellow Coeliacs in the community to be great support after my diagnosis.
It can get you down sometimes, but I try to focus on he fact that I have more energy and spend less time around porcelain.
Coeliac Australia recommend diagnosis as soon as possible, without proper diagnosis and a strict gluten-free diet, coeliac disease can lead to severe long-term health complications.
The disease is a lifelong diagnosis; if gluten is reintroduced to the diet, relapse will occur, this Coeliac Awareness Week offers opportunities for everyone, and conversation helps bring coeliac disease into the spotlight.